Early Abortion Looks Nothing Like What You’ve Been Told
Jewel is a student in her early 20s who lives in Texas. When her doctor confirmed she was pregnant, Jewel felt panicked. She knew it wasn’t the right time for her to have a child, and that abortion was illegal in her state.
Fortunately, Jewel had resources. After doing her research, she packed a bag and flew to New York City, where her sister lives. From there, the two women came to see one of us — Joan Fleischman, a family medicine doctor who has been providing abortions in her small practice in New York City for over 20 years.
Jewel, who asked to be identified by her middle name, told Dr. Fleischman about her experience in Texas. Medical staff members “were trying to push a happy pregnancy, while I was miserable and crying,” she said. Jewel sensed her doctor was afraid to even talk about other options because the doctor feared losing her license.
Dr. Fleischman performed an ultrasound, which dated the pregnancy between five and six weeks. She discussed Jewel’s options and, after confirming that Jewel wanted to end the pregnancy, completed a manual uterine aspiration procedure. This method uses a hand-held device and takes a few minutes to complete in a regular exam room.
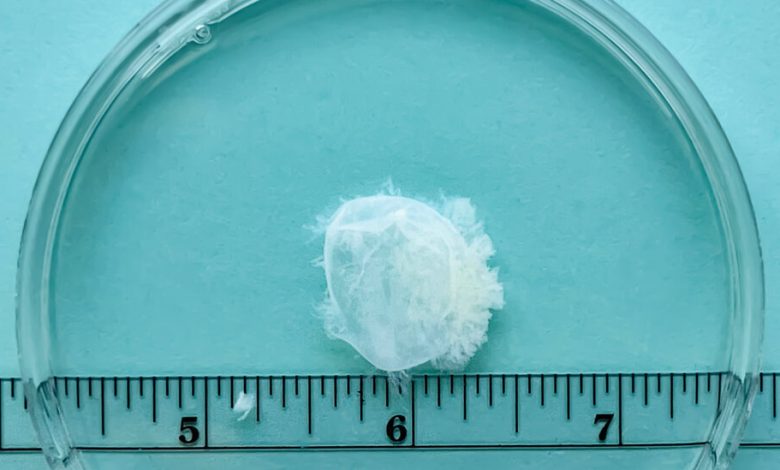
Dr. Fleischman then conducted a routine tissue examination. This involves rinsing the tissue with water using a fine sieve. She identified decidual tissue, or uterine lining, as well as a gestational sac, the visible evidence of the pregnancy. At this stage of pregnancy, the embryo is not typically visible to the naked eye.
Afterward, she offered to show Jewel the early pregnancy tissue. Jewel told Dr. Fleischman that it wasn’t what she expected. “I thought you were going to bring in something that was shaped like a little fetus or something, and it was not that at all,” Jewel said.






Early pregnancy tissue after manual uterine aspiration procedures for abortion. The first image shows fragments of uterine lining (decidua). The next images show the pregnancy tissue (gestational sacs) from five weeks through nine weeks of pregnancy. Credit…My Abortion Network
Primary care clinicians like us who provide early abortions in their practices have long known that the pregnancy tissue we remove does not look like what most people expect. After Roe v. Wade was overturned last summer in Dobbs v. Jackson Women’s Health Organization and early pregnancy termination was banned across more than a dozen states, we felt it was important to make this information public and show the images we have seen more widely.
It’s important to us to counter medical misinformation related to early pregnancy because about 80 percent of abortions in the United States occur at nine weeks or earlier. So much of the imagery that people see about abortion comes from abortion opponents who have spent decades spreading misleading fetal imagery to further their cause.
Last fall, as members of the MYA (My Abortion) Network, a clinician-led organization dedicated to educating people about abortion and expanding early abortion services into primary care settings, we launched a multimedia project to provide accurate information regarding early pregnancy tissue after abortion.
The Guardian published our first photos on Oct. 19; they went viral, appearing in media outlets and getting shared widely on social media.
Many people, even those who support abortion rights, did not believe the photos were accurate. Some insisted we had deliberately removed the embryos before taking the photos. The images weren’t consistent with those often seen in embryological textbooks, magnified on ultrasounds or used in anti-abortion propaganda; these enlarged images are not what you see with the naked eye after an abortion. A Stanford gynecologic pathologist has validated our photos, but many people could not believe the pictures were presented unaltered.
We weren’t surprised by the vitriol. We knew we’d face pushback. While we have long felt comfortable showing our patients the pregnancy tissue after an abortion, we went through serious consideration before making the images public on our website. We did not want our message to undermine our unequivocal support for patients who make this decision at later stages when there is a visible embryo or fetus.
We also recognized that people taking abortion pills or having miscarriages might find the images confusing because they don’t show the blood passed out of the body. And, of course, someone who has had a miscarriage after a desired pregnancy might feel considerable sadness when viewing the photos.
But showing these images is vital to counter misinformation, not only for patients but for our colleagues as well. Dr. Jeffrey Levine is a professor of family medicine and director of reproductive and gender health programs at Rutgers Robert Wood Johnson Medical School. He’s been teaching abortion care to fellows, residents and medical students for nearly two decades.
“When we examine the tissue after a procedure, everyone is consistently surprised. They expect to see an embryo, fetus or at least some body parts,” he told us, describing the students’ experience as “underwhelmed.”
But our primary daily work, of course, is with patients. And when our patients look at the tissue, it often makes them realize how much guilt or even shame they have internalized from society’s judgment in making this deeply personal decision.
Relief was how Jewel experienced seeing the pregnancy tissue. “I was really scared about all the horror stories and the trauma. The anxiety of coming here was worse than actually going through it,” she told Dr. Fleischman.
In many ways, medical care related to abortion has never been more straightforward. And we know abortion is an important part of primary care and could be widely available in mainstream practice settings — if the Dobbs decision hadn’t suddenly thrust many of our colleagues in states across the country into jeopardy.
Instead, we find ourselves in a country divided by politics rather than by patient need. Ensuring that our patients, colleagues and the general public have clear, objective information about abortion is critical for patients to get the care they deserve.
Erika Bliss is a family physician who provides primary care and telehealth medication abortion services through her private practice in Washington State. Joan Fleischman is a family physician who provides medication abortion and manual uterine aspiration at her practice, Early Options, in New York. Michele Gomez is a family physician who provides and teaches medication abortion and manual uterine aspiration in California. They are co-founders of the MYA Network.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips. And here’s our email: [email protected].
Follow The New York Times Opinion section on Facebook, Twitter (@NYTopinion) and Instagram.
